Case studies
See how the Auryon System worked in real practice with diverse lesion types.
These case study outcomes are unique to the individual patient undergoing atherectomy procedures under the care of qualified healthcare professionals trained in the use of the Auryon System. Individual results may vary.
See how the Auryon System was used to ablate a total occlusion in the popliteal artery after unsuccessful attempts with crossing catheters.
Introduction
Critical limb ischemia (CLI) affects 2.0 to 3.4 million people in the United States, leading to high amputation and mortality rates. The quality of life of a patient with CLI is severely impaired and is worse than congestive heart failure or advanced chronic obstructive pulmonary disease. CLI is on the rise, particularly with the increase in the prevalence of obesity and diabetes. Unfortunately, a large number of patients undergo amputation with no vascular evaluation, despite data that shows that revascularization can be quite effective in saving the ischemic limb.1-5
CLI quite often presents with total occlusions in the lower extremity vessels. This poses a challenge to treat these arteries with endovascular techniques. Multiple accesses are quite often needed along with a variety of crossing catheters and wires. Vessel prepping with atherectomy catheters and specialty balloons is regularly needed because of the long diffuse calcified lesions. Recently the pedal access has gained popularity to treat these lesions because the distal cap is generally easier to cross and, therefore, improves the success rate of a successful procedure.6 Treatment via a pedal approach is partially limited by the maximum size of the sheath that can be placed in the pedal arteries. Atherectomy devices, such as the excimer laser and orbital atherectomy, have been used from a pedal approach. Herein, we present a case using the Auryon System to retrogradely treat a totally occluded popliteal artery using a pedal access.
The Auryon System7,8 has a 355 nm wavelength with shorter pulse width (10-25 ns) leading to high laser power making it effective to tackle severe calcium. The longer wavelength allows a higher absorption of the laser photons by lesion and reduces its penetration length. The longer wavelength also has an advantage in reducing the chance of perforation. The Auryon System has a built-in aspiration system for the 2.0mm and 2.35mm laser catheters preventing distal embolization as seen in the EX-PAD-03 IDE study. The 0.9mm and 1.5mm lasers do not have an aspiration system and are best suited for tibial vessels or crossing severe calcified occlusions.
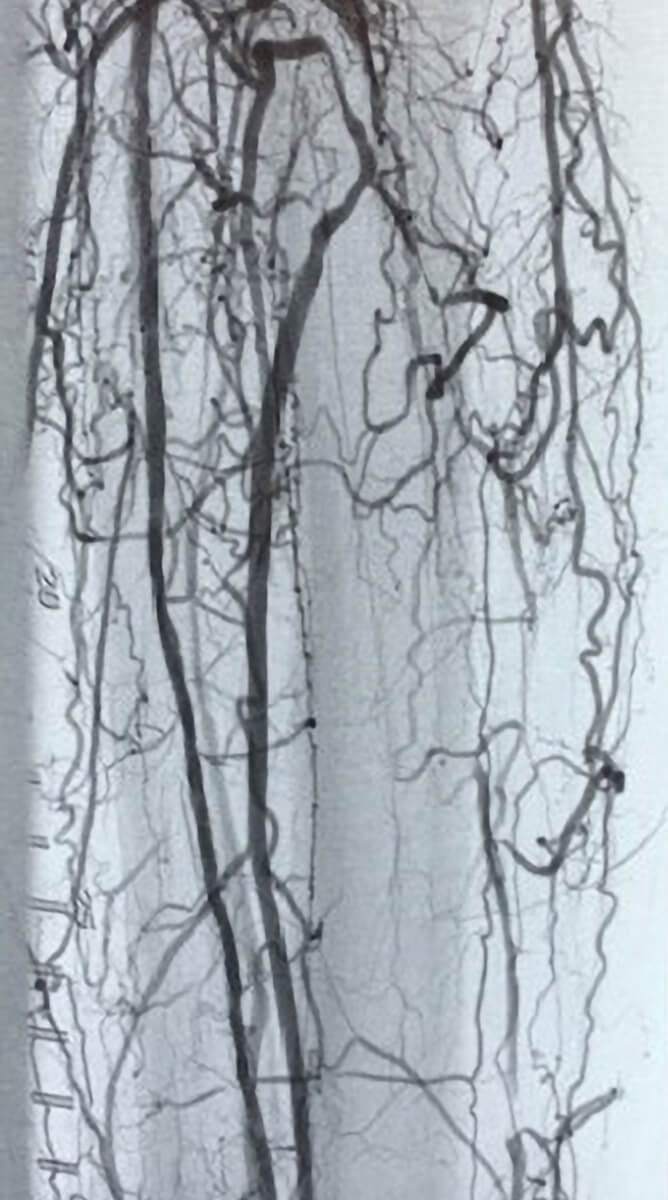
Patient history
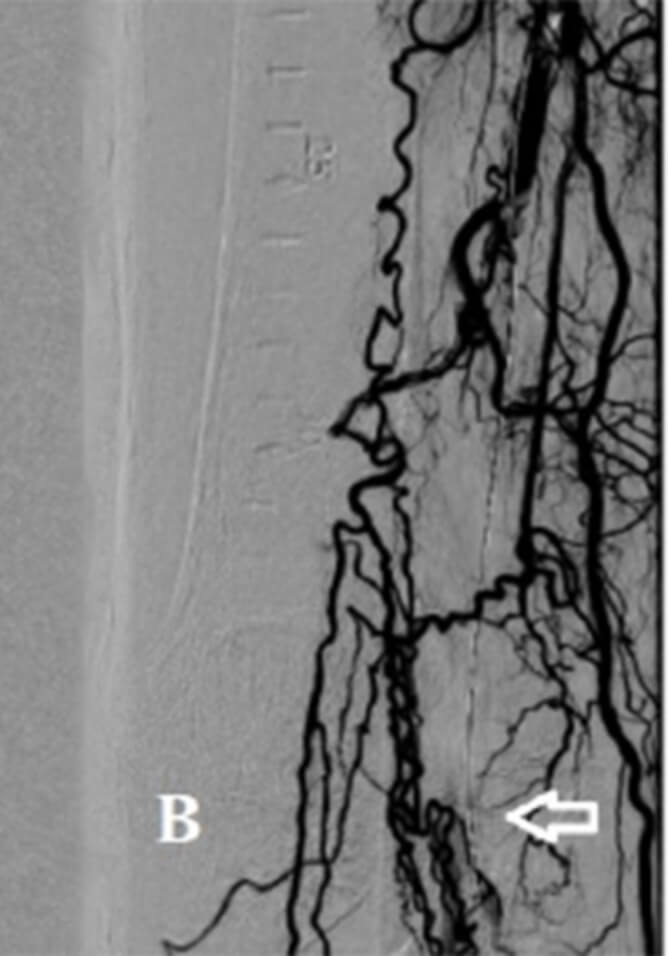
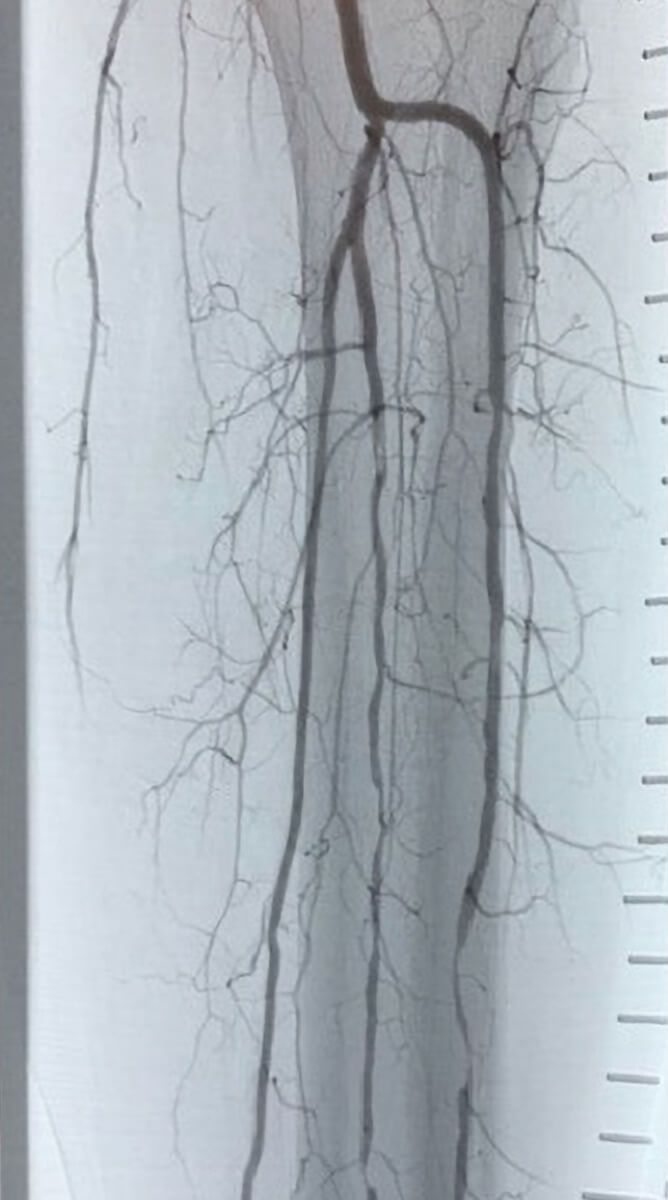
A 83-year-old male with past medical history of hypertension, hyperlipidemia, diabetes mellitus, coronary artery disease, ischemic cardiomyopathy, and peripheral arterial disease presented to the cath lab with ulcerations on his medial ankle and rest foot throbbing at night. He also has been limited in his activity because of calf muscle pains bilaterally, worse on the right. Patient underwent angiography that showed total occlusions of his right superficial femoral artery (SFA) and popliteal artery (P2 and proximal P3 segments) (figure 1A, B). Several attempts were made to antegradely recanalize these occlusions via the contralateral left common femoral artery (CFA) approach through a 7F destination sheet. These were unsuccessful despite the use of crossing catheters and crossing wires including the Astato 40 (Terumo) and 0.018” CXI crossing catheter (Cook Medical). The left posterior tibialis was then engaged with a 6F slender sheath under ultrasound guidance. Using the 0.018” CXI crossing catheter and the Astato wire, we were able to cross retrogradely the total occlusions via this retrograde pedal access. Intravascular Ultrasound (IVUS) was performed and confirmed the intraluminal position of the wire (Figure 2A). The 1.5mm Auryon catheter was then used (Figure 1C) and ablated the occlusion segment (Figure 2B). This was followed by adjunctive balloon angioplasty 6.0x150mm for 3 minutes. This showed good results in the popliteal but a wider flap dissection was noted in the left superficial femoral artery (SFA). Bailout stenting with Eluvia (Boston) stents 7.0x120mm was then performed into the distal left SFA and extended to the proximal popliteal with less than 10% residual narrowing covering the treated area (Figure 1D, 2C). The slender sheath was then removed, and hemostasis was accomplished by manual compression and transient low-pressure balloon occlusion of the left posterior tibial (PT) at the access site. The left CFA sheath was then removed and the perclose system (Abbott) was deployed successfully for good hemostasis.
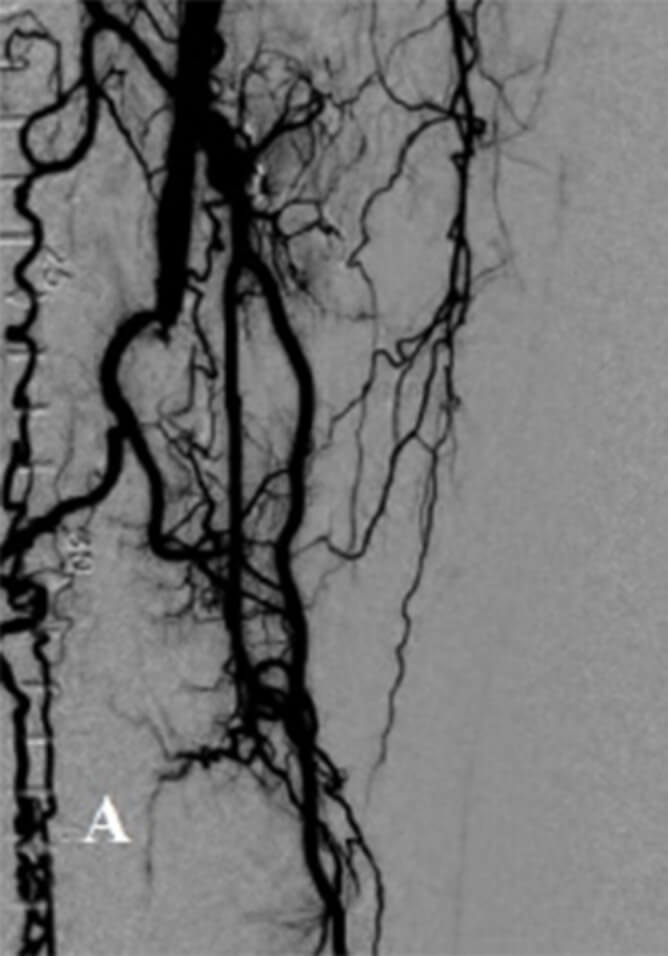
PRE AURYON LASER CTO IN THE SFA
PRE AURYON LASER CTO POPLITEAL

1.5mm AURYON LASER

POST AURYON LASER PTA RESULTS POPLITEAL ARTERY
PRE AURYON LASER IVUS SHOWING CTO AND INTRALUMINAL POSITION OF WIRE
IVUS IMAGE POST AURYON LASER IN THE POPLITEAL ARTERY
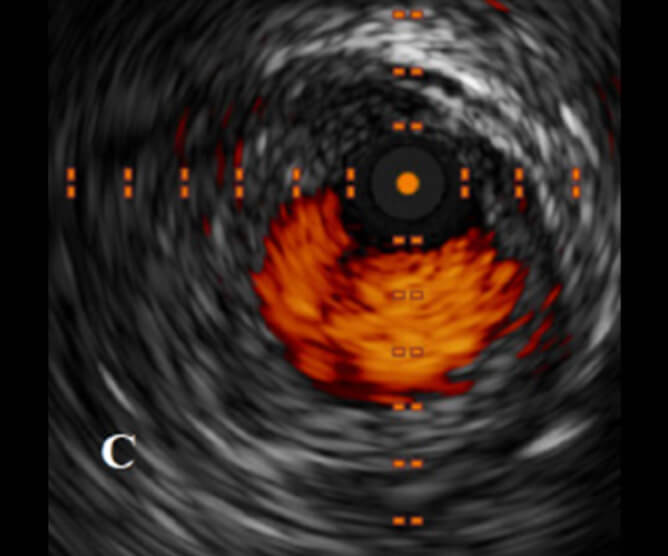
IVUS POST AURYON LASER AND PTA IN THE POPLITEAL ARTERY
Procedure notes
In this case we show the application of the Auryon System using a pedal access with successful outcome. The 1.5mm Auryon catheter can be used through a tibial vessel and appears to be effective in debulking the distal SFA/popliteal. The wire crossing via the retrograde approach was intraluminal as confirmed by IVUS. The proximal portion of the vessel however was subjected to several attempts to cross the occlusion antegradely which could have partially accounted for the dissection plane. The Auryon System has a longer wavelength (355 nm) which reduces the depth of penetration of the light. This minimizes dissections. The I-Dissection B laser study (Auryon Laser) is currently investigating the degree (depth and arc) of dissections with the Auryon System. In the IDE study, the Auryon System showed no limiting dissections and a low target lesion revascularization at 6 months (<5%). Deeper dissections are likely to cause restenosis particularly when the adventitia is involved.
References 1. Hiatt WR, Hoag S, Hamman RF. Effect of diagnostic criteria on the prevalence of peripheral arterial disease. The San Luis Valley Diabetes Study. Circulation. 1995;91(5):1472-1479. 2. Yost M. PAD Costs Economics Amputation Costs Economics, Critical Limb Ischemia, Chronic Venous Disease, Venous Ulcers, Chronic Venus Insufficiency – CLI US Supplement 2016The Sage Group. 3. Nehler MR, Duval S, Diao L, Annex BH, Hiatt WR, Rogers K, et al. Epidemiology of peripheral arterial disease and critical limb ischemia in an insured national population. J Vasc Surg. 2014;60(3):686-695.e2. 4. Bhatt D. 2005. REACH (Reduction of Atherothrombosis for Continued Health) registry. American College of Cardiology Annual Scientific Session, March 8, 2005. 5. Shammas NW. Epidemiology, classification, and modifiable risk factors of peripheral arterial disease. Vasc Health Risk Manag. 2007;3(2):229-234. 6. Radaideh Q, Shammas NW. When pedal access is the only way to save a limb! Int J Angiol. 2020;29(3):205-209. 7. Shammas NW, Chandra P, Brodmann M, et al. Acute and 30-day safety and effectiveness evaluation of Eximo Medical’s B-Laser™, a novel atherectomy device, in subjects affected with infrainguinal peripheral arterial disease: results of the EX-PAD-03 trial. Cardiovasc Revasc Med. 2020;21(1):86-92. doi:10.1016./j.carrev.2018.11.022. 8. Rundback J, Chandra P, Brodmann M, et al. Novel laser-based catheter for peripheral atherectomy: 6-month results from the Eximo Medical B-Laser™ IDE study. Catheter Cardiovasc Interv. 2019;94(7):1010-1017.
See how the Auryon System was used to restore patency through atherectomy of the tibial and peroneal arteries.
Patient history
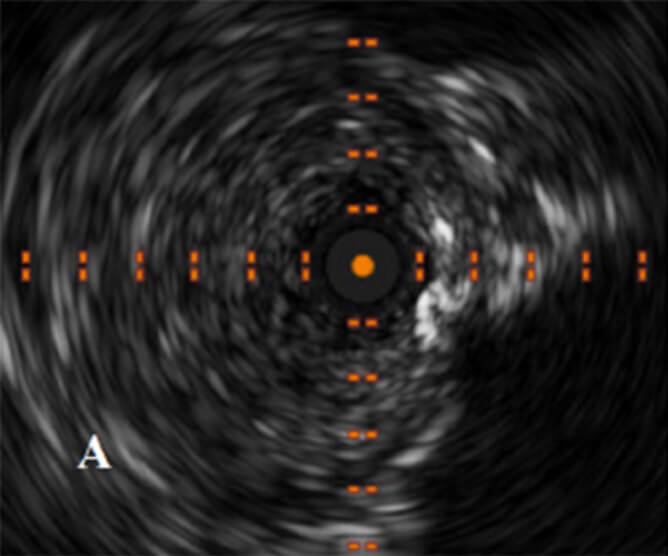
A 50-year-old male with a past medical history of hypertension, hyperlipidemia, insulin-dependent diabetes mellitus, presented with a chronic ulcer to left great toe which was cool to the touch. The patient was recently hospitalized, was seen by podiatry for wound care, and presented wearing a boot on the left foot. Stated that he has been experiencing a ‘pulsating’ pain in his foot. The decision was made to proceed with a PTA procedure in an attempt to improve blood flow and wound healing.
He was brought to the cardiac catheterization lab where diagnostic angiography showed a heavily calcified SFA. The left popliteal artery in the P1 segment had a flow-limiting lesion with approximately 15 to 20 mmHg gradient across the lesion. The left anterior tibial artery was a moderate-size vessel with a focal 50% stenotic lesion and a tubular 50% to 60% stenotic lesion. The left peroneal artery revealed a 50% stenosis proximally with a subtotal 99% stenosis in the mid to distal aspect and left posterior tibial artery revealed a 20% diffuse stenosis.
Due to the angiographic findings, the decision was made to proceed with improving inflow and outflow as well as improving flow to the digital vessels.
Pre-treatment with the Auryon System
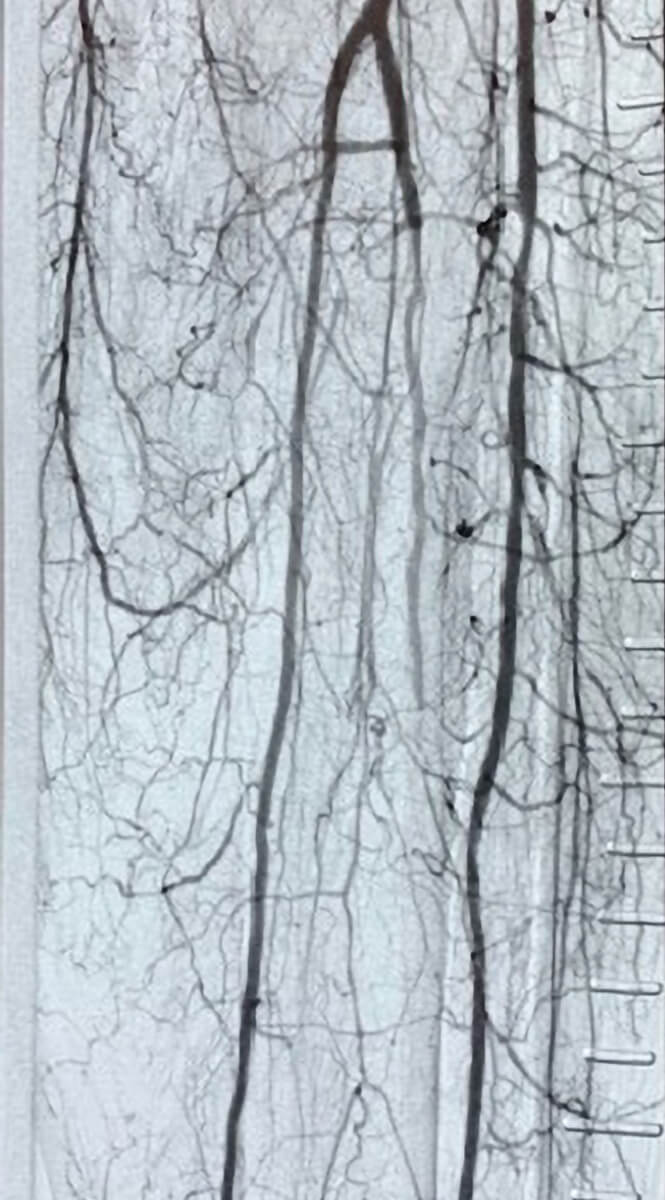
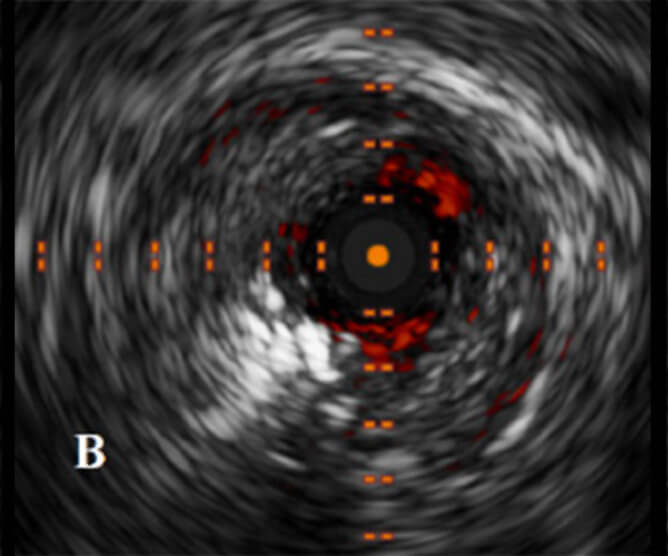
Post-treatment with the Auryon System
Procedure notes
After angiography was performed, excellent flow into the digital vessels to the dorsalis pedis artery was confirmed. Attention was given to improving flow in the left anterior tibial artery. A second SION black guide wire (Asahi Intecc, Seto, Japan) was then advanced, and the 1.5 x 8 Apex over-the-wire balloon (Boston Scientific, Marlborough, MA) was advanced across the lesions in the left peroneal artery into the distal vessel. The vessel tapered significantly at the level of the ankle, with very poor outflow. At this aspect, a 0.9 mm AURYON laser atherectomy catheter [(AURYON Atherectomy System, AngioDynamics, Queensbury, NY)] was inserted over the wire and advanced to the left anterior tibial artery. Atherectomy was performed at 50 mJ/cm2. The 0.9 mm AURYON laser atherectomy catheter was then exchanged onto the wire of the peroneal artery for 50 mJ/cm2. After atherectomy was performed, the AURYON catheter was exchanged for an Armada 14 XT OTW 2 mm x 200 mm balloon (Abbott Vascular Inc., Redwood City, CA) which was inserted into the left peroneal artery and inflated to 5 atmospheres for 2 minutes. After balloon angioplasty was performed, there was significant improvement in flow distally. A 6 mm x 120 mm Chocolate balloon catheter, Chocolate OTW Percutaneous Transluminal Angioplasty (PTA) Balloon (Medtronic Corporation, Minneapolis, MN), was inserted in the left peroneal artery and gently inflated to 5 atmospheres for 2 minutes. There was no gradient across the peroneal artery post inflation, and final angiography revealed less than 10% stenosis of the popliteal artery. There were sequential 20% stenotic lesions of the left anterior tibial artery.
The proximal peroneal artery and mid-peroneal artery revealed excellent flow. There was a taper to a very small caliber vessel with poor distal flow and small caliber vessels. There was now excellent flow into all the digital vessels and confirmation of excellent flow into both the medial and lateral aspects of the 1st digit. The patient will continue with clopidogrel (Plavix, Sanofi-Aventis US LLC, Bridgewater, NJ) and will be given a 300 mg dose overnight.
See how the Auryon System was used to restore patency through atherectomy of the anterior tibial artery and the popliteal artery in 1 pass.
Patient history
A 61-year-old male with a past medical history of coronary artery disease, hypertension, diabetes mellitus type 2, diabetic foot ulcers of the plantar forefoot of both feet (for 2 years) and peripheral neuropathy. The patient presented with bilateral swelling and pain in both feet which is usually controlled with Gabapentin (Amneal Pharmaceuticals LLC, Bridgewater, NJ) and Ultram (Tramadol, Janssen Pharmaceuticals, Inc., Raritan, NJ). On the day of admission both feet were more swollen and painful than usual and the patient self-treated with Gabapentin and Furosemide (LASIX, Pfizer, New York, NY) in hopes that the swelling would subside as well as the pain (no improvement). The patient’s pain increased until he could only walk on his heels. In agreement with podiatry the patient was referred to the Emergency Department and was subsequently admitted. A noninvasive imaging study demonstrated severe abnormalities and the patient was in extreme pain as previously reported.
The patient was brought to the cardiac catheterization lab where diagnostic angiography revealed bilateral iliac arteries with luminal irregularities. Bilateral superficial arteries were severely calcified with approximately 20% to 30% stenosis and diffuse disease. The right popliteal artery revealed a 60% stenosis in the mid-segment, and left popliteal artery revealed 50% stenosis with occlusion in the distal aspect. The right anterior tibial artery was completely occluded with no significant reconstitution and right tibioperoneal trunk was occluded with reconstitution of the peroneal artery. There was 100% total chronic total occlusion of the right popliteal and right posterior tibial arteries. All 3 tibial vessels appeared occluded on the left lower extremity with possible washout.
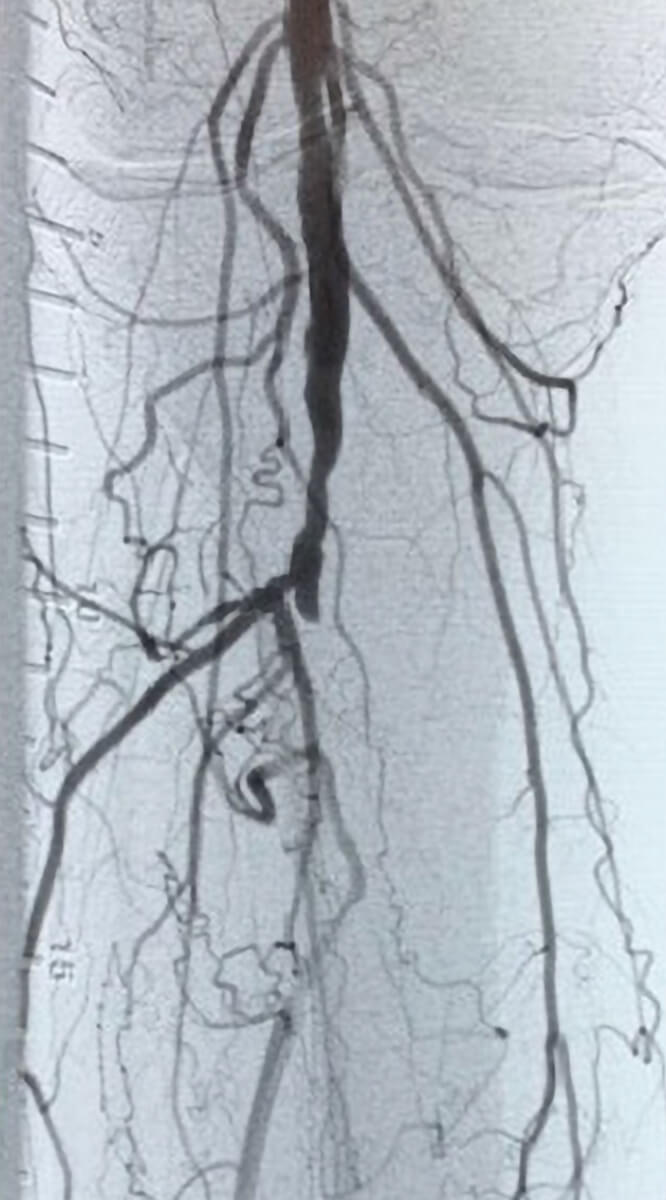
Pre-treatment with the Auryon System
Post-treatment with the Auryon System